- October 17, 2025
Table of Contents
ToggleJaundice In Newborns
One of the most common conditions neonatologists deal is neonatal jaundice, or NNJ medical abbreviation, which causes a yellowing of the skin and yellowing your baby’s eyes (sclera) . This occurs in many babies born at term and is even more common in preterm infants. It happens due to a buildup of bilirubin. Understanding the bilirubin normal value in newborn infants is the key. The American Academy of Pediatrics (AAP) emphasizes that this isn’t a single number but a dynamic value based on your baby’s age in hours. This jaundice develops when a newborn’s liver, which is still maturing, can’t process bilirubin quickly enough. Most cases are mild, but high levels need prompt attention to reduce the risk of developing complications.
When to Call the Doctor: 5 Clinical Symptoms of Neonatal Jaundice
Monitor your newborn closely for these 5 key symptoms of jaundice. Contact your baby’s doctor immediately if you notice:
- Yellowing of the Skin and Body: A distinct yellow tint spreading on the skin, abdomen, arms, or legs.
- Yellowing of the Eyes: The whites of your baby’s eyes (sclera) appear yellow.
- Extreme Lethargy: Your baby is hard to wake, unusually sleepy, or lacks energy.
- Poor Feeding: Difficulty breastfeeding or taking formula, with a noticeable decrease in intake.
- Unusual Fussiness: Your baby is excessively fussy, irritable, or difficult to console.
Early detection is crucial. If you observe any of these jaundice signs, do not hesitate to call your pediatrician for an immediate evaluation.
Bilirubin Normal Value and the Essential SBR Test
Following AAP guidelines, we don’t rely on a single “normal” bilirubin normal value. Instead, we use an hour-specific bilirubin nomogram to assess risk. The SBR test (Serum Bilirubin Test) is crucial for this. This simple blood test gives us the precise bilirubin level to plot on the chart below, determining if your baby is in a low-risk or high-risk zone. This is the cornerstone of modern, proactive management.
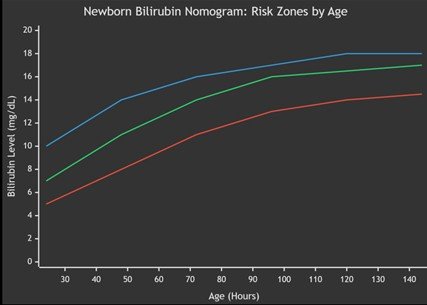
The graph above illustrates the key concept: the threshold for concern changes dramatically in the first days of life. The SBR test result places your baby in a risk zone, guiding our decisions. You might hear the term Pila Yarkan, which translates to “yellow disease” in some languages—it’s the same condition, underscoring its global nature.
What Causes Neonatal Jaundice? The AAP Framework
Jaundice stems from issues in three areas: bilirubin production, processing, or elimination. The AAP’s systematic approach helps us identify the cause quickly. The chart below outlines the major categories:
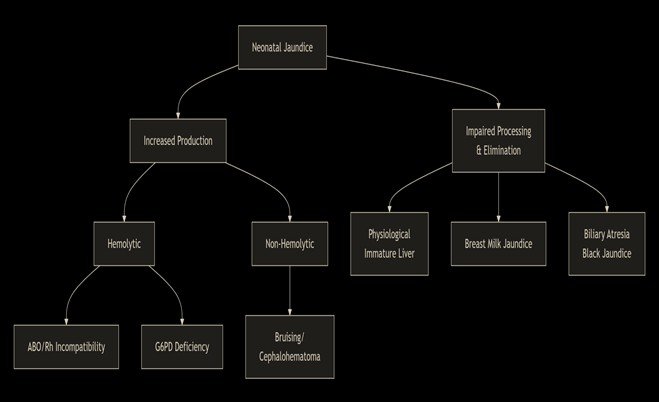
- Increased Production: This includes hemolytic causes like ABO incompatibility, where a mother’s antibodies attack the baby’s red blood cells, leading to rapid bilirubin release.
- Impaired Processing: The most common scenario is “physiological jaundice,” where the newborn’s liver is simply immature. This also includes breast milk jaundice.
- Elimination Problems: Serious but rare conditions like biliary atresia (sometimes referred to as black jaundice) prevent bilirubin from being excreted.
Is Jaundice Transmittable? A Clear Answer
A very common question is, “Is jaundice contagious?” Let me be unequivocal: Jaundice is not transmittable. The yellow color itself cannot be “caught” or spread. It is a symptom, not a disease. While a rare underlying infection causing jaundice might be contagious, the jaundice is not. It is not spreadable through contact.
The Sunlight Question: Why AAP Guidelines Advise Against Direct Sun Exposure
How is Jaundice in Babies Treated? Effective Methods Explained
Most cases of newborn jaundice are mild and resolve on their own. However, when bilirubin levels are high, prompt treatment is essential to prevent complications. Here are the primary methods used to treat jaundice in newborns.
Phototherapy (Light Therapy)
This is the most common and effective treatment.
- Your baby is placed undressed under special blue-spectrum lights.
- These lights help your baby’s body break down bilirubin so it can be easily removed.
- Treatment is typically done in the hospital, but home phototherapy units are sometimes an option.
Increased Feeding and Hydration
For mild cases, simple dietary changes can help.
- More Frequent Feedings: Whether breastfeeding or formula-feeding, increasing the frequency helps promote bowel movements, which is the main way bilirubin is excreted.
- Supplementation: In some breastfed babies, a doctor may recommend supplementing with formula to ensure adequate hydration and calorie intake.
Exchange Transfusion
This is a rare but critical procedure for severe, emergency-level jaundice.
- It involves slowly removing the baby’s blood and replacing it with donor blood.
- This rapidly lowers bilirubin levels and is a life-saving intervention.
Important Note: The choice of treatment depends entirely on your baby’s bilirubin level, age, and overall health. Your pediatrician will determine the safest and most effective approach.
Conclusion: Empowered and Informed Care
In summary, neonatal jaundice is a common part of the newborn journey. By understanding the neonatal total bilirubin normal range as a dynamic, hour-specific value, you are better equipped to partner with your healthcare team. Remember, jaundice is not contagious, and its management is highly effective. Always follow the guidance of your pediatrician, who uses evidence-based AAP guidelines to ensure your baby receives the safest care, from monitoring with the SBR test to providing medical phototherapy if needed. This proactive approach ensures a healthy start for your child.